HPV vaccine can protect against cervical cancer
Parents and guardians of teenage girls are being reminded of the importance of girls receiving the Human Papilloma Virus (HPV) vaccine.
Cervical cancer is the fourth most common cancer in women worldwide but the HPV vaccine can help protect against it, reducing the risk of getting cervical cancer by over 70%
The vaccine is offered to girls in year 9, with a chance to catch up on any missed doses in year 10. Letters are being sent to parents and guardians of girls who are eligible, with information on how they can receive it this school term.
All girls who have their first dose before the age of 15 only need two doses in total, at least six months apart.
It is estimated that the level of protection offered by the vaccine will last for at least 10 years.
Though uptake of the vaccine has fallen slightly recently, it is relatively high in Northern Ireland, but there are still girls who are not benefitting from this free, simple opportunity to do something which could save their life.
Dr Lucy Jessop, Consultant in Health Protection at the PHA, said: “Cervical cancer can kill so we are fortunate to be able to offer teenage girls the HPV vaccine to help protect against it. I would urge all parents or guardians to talk to their daughters about the importance of getting the vaccine and ensure that all eligible girls complete the course of vaccines when offered in school this term.
“Even though the vaccine has only been available in the UK for nine years, it is very encouraging that decreases in pre-cancerous lesions in the cervix and in genital warts have already been seen.”
Each year around 95 women are diagnosed with cervical cancer in Northern Ireland with an average of 22 women dying from the disease.
In addition, 1,225 cases of cervical cancer in situ are diagnosed each year. This is where some cells of the cervix have pre-cancerous changes, which could lead to cancer if not treated.
Persistent infection by high-risk HPV types is detectable in more than 99% of cancers. Of these high risks types, HPV 16 and HPV 18, which the vaccine can protect against, are together responsible for 75% of all cervical cancer types in Europe.
If parents have any questions about the vaccine, they can find more information on the PHA website www.pha.site/hpv or they can contact their school nurse directly.
Ends
Notes to editors:
- More than 80 million girls and women have received the HPV vaccine worldwide and it has a good safety record.
- The HPV vaccine was introduced into the UK in 2008, with a change to using Gardasil vaccine in 2012 which prevents against HPV 16 and 18 as well as types 6 and 11 which cause the majority of cases of genital warts.
- The vaccine’s effects on the disease prevention are already being seen in countries across the world. In England, among teenage females aged 16 to 18 years there has already been a significant decrease in the prevalence of the two main HPV types that can cause cervical cancer, with a 60% decrease in HPV 16 and a 73% in HPV 18.
Scottish researchers have shown a decline in HPV16 and 18 as well as, in three other HPV types linked to cancer (types 31, 33 and 45) probably due to cross-protection.
The number of precancerous lesions in the cervix has already fallen by over 50% since the programme began in Australia, Denmark and Scotland. - These vaccines do not protect against all HPV types that cause cervical cancer, so vaccinated girls need to continue to attend for cervical screening when they are invited. However, there is evidence of some protection against some of these types that are not in the vaccines (cross protection).
- A recent report from Northern Ireland also showed a decrease of 48% for genital warts in 16-19 year old girls.
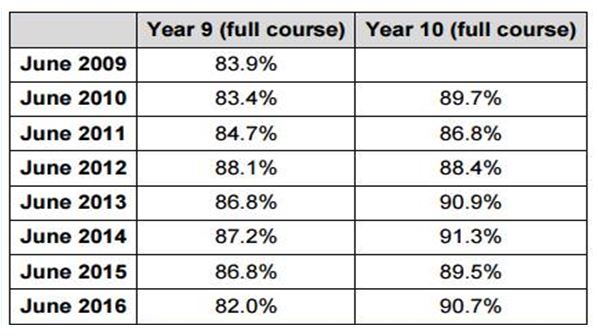
- As of June 2017 the vaccine uptake in Year 9 was 74.6% and in Year 10 uptake was 89.6%
- Uptake figures for HPV vaccine 2009-2016 can be found in the following table: