Professor Hugo Van Woerden, PHA Director of Public Health and Dr Damian Bennett, Consultant in Public Health Medicine explain reporting differences by the Public Health Agency and the Northern Ireland Statistics and Research Agency for COVID-19 related deaths. To view our complete series of COVID-19 blogs, click here.

Understandably, there has been some confusion regarding COVID-19 death reporting by different organisations. This blog describes what is collected on a daily basis by the Public Health Agency (PHA) and some of the differences with what is reported weekly by the Northern Ireland Statistics and Research Agency (NISRA). We recognise that the details of data flows is a niche topic, and not one that keeps everyone awake at night! But here goes.
NISRA reports
The traditional method for examining the number of deaths, and the range of causes of death, takes information from death certificates that are handed into the Registrar’s Office. However, a family may take up to five days after a loved one has died to hand in the certificate. There may also be a delay between the time of a death and a laboratory results taken on that patient, which may affect whether a death is recorded in the short term as a suspected or confirmed COVID-19 death.
The death certificate contains two parts. Part 1 describes the immediate causes of death and Part 2 provides information on related conditions that may also have contributed to death. The number of deaths from COVID-19 can either be reported on the basis of a reference to COVID-19 in Part 1, or both Part 1 and Part 2.
NISRA do not report on deaths that have occurred in the preceding week because of some of these factors and their requirement to have an ‘official’ figure.
Daily reports
There are similar but different challenges with the data collected by the PHA, as we are also dependent on receiving reports of each death before we collate our daily figures, usually at 10am each day. Hospital and community recording systems were not designed to deliver in such a tight daily timeframe. The need for a new computer system to help modernise records is well recognised by the government and a new national system is planned. This will make a difference when it is installed, but such a system may take a number of years to build and the process is still in its infancy.
In summary, there is a time lag in deaths reported to the PHA as well as a time lag in the deaths reported to NISRA. This affects the completeness of any methods for ‘next day’ reports.
PHA records are normally used for internal planning purposes, where the focus is on a timely report rather than a focus on record completeness. The epidemiologists involved have a clear understanding that the short term spikes or dips may in part reflect bottlenecks in the reporting system, rather than real changes in the trend. For example, some deaths that have occurred over a weekend may not be reported until the middle of the following week, as ward clerks and other staff catch up on tasks left over by a smaller team on duty at the weekend during the rest of the week. So, totals by date of death, particularly for recent prior days, are likely to need to be updated at a later date.
Examining average deaths over a 7 day period and excluding the last few days gives a better idea of the trend in daily deaths as can be seen in the graphs below (Figures 1 and 2).
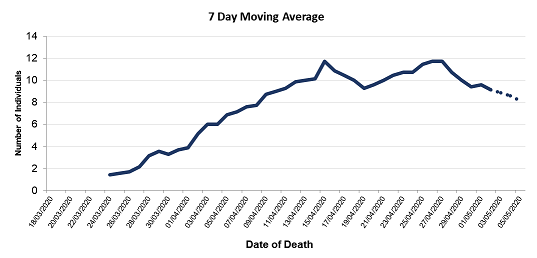
Figure 1. Reported deaths by date of death, 7 day moving average, up to 5th May (provisional)
In the graph above (Figure 1) we can see a drop in the 7 day average at the right of the graph, suggesting that reported deaths have dropped in the last few recorded days (dashed line). However, this is often due to a delay in reporting rather than real changes in the trend.
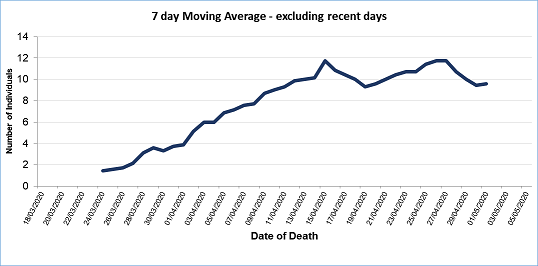
Figure 2. Reported deaths, by date of death, 7 day moving average, up to 2nd May (with axis extended to 5 May)
If we look at Figure 2 above, where we have excluded the most recent four days, we see that the 7-day average remains at an approximate steady state of about 10 deaths per day. Continued monitoring of COVID mortality data is required to see if the reduction in deaths is sustained.
An international reporting problem
This situation is not unique to Northern Ireland, and inevitably most countries will display a difference between daily reported “COVID-19 related deaths”, and “registered deaths”. There will also be differences between countries depending on their testing regimes and whether a country only reports on hospital deaths.
Adding a report on deaths from community settings can have a large impact. An example of this occurred in France on 2 April 2020, when the government announced a huge increase in the recorded deaths of 1,353 over a 24 hour period. This increase included 884 fatalities that had occurred in nursing homes in weeks preceding the announcement, but were only been formally notified on 2 April, making the large increase that day potentially misleading. Similarly, the inclusion of care home deaths in England from 29 April (which had previously only included hospital deaths) also led to a sudden jump in total daily reported COVID-19 associated deaths. In general the public health advice would be that one should avoid interpreting daily figures and should use trends instead.
Complex definitions
The definition of “COVID-19 associated death” is complex and difficult to understand. Most countries are reporting daily figures using laboratory confirmed deaths. The definition that is used for daily reporting by the PHA is: ‘any individual meeting the confirmed case definition (laboratory confirmed infection, regardless of symptom status) who has died in the 28 days after the specimen date for which a positive test result was received, whether or not COVID-19 was the cause of death’.
Gathering information to meet this definition is complex. There will be individuals who have died as a consequence of COVID-19 but who have not had a positive laboratory result. This is inevitably not picked up in the daily figures collected by the PHA, but will be recorded in the later weekly NISRA report of all certified deaths, as the NISRA reports use a different definition and a different source of information.
The daily report
The daily report draws on a variety of sources and there are several steps in collecting this data. PHA sources include reports by healthcare workers using an online form that is completed by staff in Health and Social Care Trusts and GPs. It may also occasionally include deaths reported through phone calls or email correspondence by, for example, care home managers. One source of potential inaccuracy of the data is the fact that on occasion clinical staff may be so busy that they cannot complete the online report of a death, or may take more than a day to do so.
To get the final figure that the PHA collate, the reported deaths have to be linked up to positive COVID-19 laboratory results. Again, the laboratory results can be problematic. The name used by the laboratory may be different from that given when reporting the death. For example, the form received by a laboratory may use a colloquial first name such as James, Jimmy, Jonny, or Jack, whereas a report of a death might use a more formal first name such as John. Differences such as these can make it complex and time consuming to link different data sources.
The laboratory results are not always received within a time frame that allows them to be captured in a daily report. This can mean that earlier data has to be updated. There can occasionally be difficulty with dates, for example, clarifying that the laboratory test was taken within the preceding 28 days, as the date that the sample was taken may be different from the day that the sample was received by the laboratory, which may be the one recorded in a computer system. Lots more could be said, but this perhaps illustrates some of the problems that there are working with this kind of data.
Conclusion
In summary, both the NISRA data and the data collated by the PHA on deaths rely on complex pathways and busy front line staff who may naturally prioritise urgent clinical care over some aspects of form filling. Timely data is helpful, but the result of seeking to be very timely, as the PHA does, is that such data always needs to be interpreted with caution, and needs to be regularly revised and updated.
The General Register Office (GRO) data are the most reliable source of information on deaths, including those due to COVID-19. However, it is not available in as timely a fashion.
Daily reporting on deaths from COVID-19 is primarily a guide, aiming to help inform planning systems about the spread and impact of the virus.
For those who are interested, this complex topic is also covered in a BBC piece on why COVID-19 death data can be difficult and in a report by FactCheckNI.
If you are interested in data you may want to check them out!
To view our complete series of COVID-19 blogs, click here.
