Smoking and COVID-19
What we know about the association of smoking with the COVID-19 virus, and how we in the PHA can support smoking cessation during the pandemic
Dr Claire Neill, Specialty Registrar in Public Health Medicine, Elaine Wilmot, Health Intelligence Manager, and Kelly McCartney, Health Improvement Manager, Public Health Agency
Our knowledge about COVID-19 is constantly on the increase, thanks to ongoing research in this area. Early evidence suggested that smokers may be more susceptible to serious illness from COVID-19, and may also be at increased risk of contracting the virus if they are exposed, due to repeated hand to mouth movements giving the virus more opportunities to enter the body.[i] We explore some of the emerging evidence in this area, and explain why there has never been a more important time to give up smoking and how we, in the Public Health Agency (PHA), can help support this.
What does the evidence say about COVID-19 and smoking?
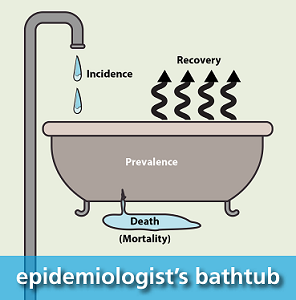
The World Health Organization (WHO) has completed an analysis of 35 peer reviewed studies on the association of smoking with COVID-19.[ii] The review found that smokers are more likely to develop severe disease from COVID-19 than non-smokers, and in hospitalised patients with COVID-19, smoking was also associated with increased severity of illness and death.
A smaller study, quoted by Public Health England (PHE) in response to the findings, suggested that smoking was a significant predictor of disease severity, with smokers being 14 times more likely to develop severe respiratory disease than non-smokers.[iii]
An additional review comparing current smokers with both ex-smokers and non-smokers included 19 studies and a total of 2,473 people with COVID-19 infection.[iv] The review found that current smokers are more likely to develop severe complications associated with the infection, when compared with former smokers and people who have never smoked.
It is an important time to consider giving up smoking, not only to reduce your risk of contracting COVID-19, but also to reduce the risk of severe disease associated with the infection.
How can we support smoking cessation during the COVID-19 pandemic?
Stopping smoking can be difficult, and we know that this is particularly the case during times of stress. Additionally, face-to-face support for smoking cessation has not been as accessible during lockdown, and the associated loss of routine or boredom may even exacerbate relapses for ex-smokers, or increased smoking behaviour in those who smoke.
The PHA commission approximately 600 specialist ‘Stop Smoking’ services across Northern Ireland, and smokers can access these services via a range of local settings including GP practices, pharmacies, hospitals, and community or voluntary groups. These services are specifically designed for smokers who are motivated and ready to quit, and who are prepared to set a quit date.
Services are provided by specialist practitioners who have received specific training to carry out this role. Smokers can avail of intensive treatment over the course of 6-12 weeks through a combination of pharmacotherapy and behavioural interventions which have proven to be the most effective mechanism to help smokers to quit. 5
Smokers are more than four times more likely to quit using this approach and to date the provision of specialist Stop Smoking Services in Northern Ireland has supported nearly 300,000 smokers to quit smoking.
In addition to specialist support, smokers interested in quitting are also able to request a ‘Quit Kit’ from the PHA’s stop smoking website. The website has been created with the involvement of smokers and ex-smokers to support people in their quit attempt. The site has information on the benefits of quitting, stop smoking aids and the current support available.
Please visit www.stopsmokingni.info for more information and to have the best chance of success in becoming smoke free.
[i] World Health Organisation. Q&A: Tobacco and COVID-19. Available from: https://www.who.int/news-room/q-a-detail/q-a-on-tobacco-and-covid-19
[ii] World Health Organisation. Smoking and Covid-19. Available from: https://www.who.int/publications-detail/smoking-and-covid-19
[iii] Public Health England. Smokers at greater risk of severe respiratory disease from COVID-19. Available from
[iv] Patanavanich R and Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine & Tobacco Research. https://doi.org/10.1093/ntr/ntaa082
5 Department of Health. Health Survey (NI): First Results 2018/2019. Department of Health: Belfast, January 2020.